
Dr. Sandra Iuliano and her team investigated whether the risk of falls and of bone and hip fractures decreased in older adults if they received additional daily servings of dairy. The results were startling: 33% fewer bone fractures, 46% fewer hip fractures and 11% fewer falls. Iuliano’s study appeared in the renowned British Medical Journal.
By Rob van Berkel
A complete diet is important for older adults, but often proves difficult to achieve. Older adults may start eating less for a variety of reasons, including illness, reduced appetite, or difficulty chewing. But just as often psychological problems (depression, grief), loneliness and dementia and the use of medication play a role. When older adults do not get enough calories and micronutrients for a long period of time, they quickly become malnourished. This can lead to a decrease in body weight and muscle mass and to an increased risk of falls and bone fractures. This while the risk of falls and bone fractures is already much higher in older adults because muscle and skeletal mass decreases with age.
Intervention in older adults
Older adults often have a low intake of the nutrients involved in good bone health and are therefore at increased risk of bone fractures. Dairy contains several nutrients that contribute to good bone health, including protein, calcium, and phosphorus. Cheese is also a good source of vitamin K2. A meta-analysis with 6 randomized controlled trials found that dairy increases bone mineral density in post-menopausal women. Another meta-analysis with 7 observational studies showed that a diet rich in dairy was associated with a 41% lower risk of low bone mineral density.
Australian study
Increasing dairy consumption in older adults may be a relatively easy, inexpensive, and safe solution to maintaining bone health. The most reliable way to investigate this is with a randomized controlled trial with a sufficient number of participants. In Australia, this exact study was conducted by Dr. Sandra Iuliano (see interview) and her team.
Two-year trial
The trial was done in 60 care settings in Australia with 7,195 older adults (n=7,195). The average age was 89 years and 68% of them were women. Because the care provided by the nursing homes had to be comparable, only nursing homes accredited by the Australian Aged-Care Accreditation Agency were included in the trial. For example, a condition of accreditation is that all older adults receive a vitamin D supplement. Other conditions for participation in the trial were:
- Residents consumed less than 2 servings of dairy per day
- Residents’ calcium intake was less than 600 mg/day
- Residents’ protein intake was less than 1 gram per kg of body weight per day
The 60 nursing homes were divided into 2 groups (see Table 1). In one group, residents continued to receive their usual menu (control group); in the other group, dairy intake was increased (dairy group). The nursing homes involved achieved this increase in dairy intake by changing recipes, enriching milk with milk powder, or by offering dairy desserts and snacks instead of foods with a lower nutritional value. Residents with lactose intolerance were offered lactose-free dairy products. The total trial lasted two years and randomization took place per nursing home. To maintain the number of individuals in each group, participants who dropped out due to discharge or death were replaced by other residents.
The primary outcome measure of the study was the occurrence of bone fractures. Secondary outcomes were incidence of falls and changes in bone morphology and biochemical parameters. Tertiary outcomes included mortality and changes in body composition.
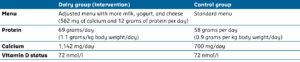
Table 1: Differences and similarities between the dairy group and the control group.
Results
After two years of the trial, of the 60 nursing homes, 54 were still involved, 25 of which were in the dairy group and 29 in the control group. Three nursing homes in the dairy groups did not go through with the trial. After 15 and 20 months, respectively, two nursing homes were closed, but this occurred after randomization for the trial. One nursing home in the control group changed owners.
Dietary changes
In the dairy group, dairy intake went up from 2 to 3.5 servings per day (Figure 1). One serving consisted of 250 ml of milk, 200 grams of yogurt, or 40 grams of cheese. Thus, the increase in dairy is equivalent to, for example, 250 ml of milk and 100 grams of yogurt or 20 grams of cheese. The higher dairy consumption led to an increase in protein and calcium intake (Table 1). No differences in calorie intake were found for the total diet.
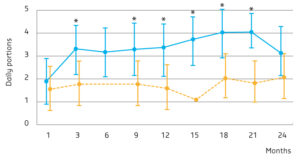
Figure 1: Average dairy consumption of the dairy group and the control group at baseline and during the 2-year trial period.Orange: control group, blue: intervention group.
* Significant difference compared to the control group (p<0.05).
Bone fractures, falls, and mortality
After an average follow-up of 12.6 months, 324 incidences of bone fractures had occurred. Of these, 121 (3.7%) bone fractures occurred in the dairy group and 203 (5.2%) in the control group. This means that the dairy intervention led to a 33% reduced risk of bone fractures (HR: 0.67; 95% BI: 0.48-0.93) (Figure 2). All but one of the bone fractures were due to a fall.
A 46% reduced risk was found for hip fractures (HR: 0.54, 95% BI: 0.35-0.83) (Figure 2). Reduced risks were found from 5 months onwards. This means that one bone fracture and one hip fracture per 52 and 82 older adults, respectively, are prevented when dairy intake is increased similar to the dairy intervention in the trial.
The cumulative incidence of falls was 57% (n=1,879) in the dairy group and 62% (n=2,423) in the control group. The dairy intervention thus led to an 11% reduced risk of falls (HR: 0.89; 95% BI: 0.78-0.98) (Figure 2). This means that one fall is prevented per 17 older adults when dairy intake is increased.
No difference in mortality was found between the two groups (Figure 2).
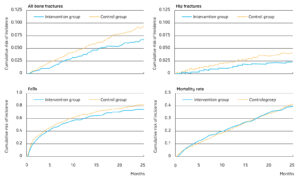
Figure 2: Cumulative risks of bone fractures, hip fractures, fall incidence, and mortality in the dairy group and the control group.
Bone morphology, biochemical parameters, and body composition
Thanks to more complex measurements in a subgroup, this trial also looked at bone morphology, biochemical parameters, and body composition (Table 2). Measurements took place at baseline and after 12 months. A clear difference in CTX (a measure of bone degradation) and IGF-1 was observed between the groups. In addition, participants in the dairy group had higher average bone mineral density of the lumbar vertebra and distal radius. Whereas the control group had lost an average of 1.4 kg per person, the dairy group remained at the same weight. Weight loss in the control group consisted of 0.3 kg of lean body mass in the arms and legs and 0.8 kg of fat body mass.
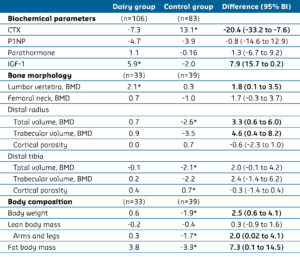
Table 2: Mean percentage change in biochemical parameters, bone morphology, and body composition from baseline to month 12.
CTX = C-terminal telopeptide (marker for bone degradation), P1NP = Total procollagen type 1 N-terminal propeptide (marker for bone formation), IGF-1 = Insulin-like growth factor 1, BMD = Bone mineral density.
* Significant difference compared to baseline within group (p<0.05).
Bold = Significant difference between the two groups (p<0.05).
Beneficial effect
At the start of the study, all older adults had lower intakes of protein and calcium than recommended. The authors indicate that the beneficial effect would have been less likely had the older adults eaten according to the recommendations. One explanation for the beneficial effects of the dairy intervention is that it slowed down bone loss and reduced microstructural decline. A meta-analysis into the effect of supplementation with calcium (with or without vitamin D) on incidence of bone fractures in people over 50 shows a similar picture. A beneficial effect was also found at a previous calcium intake of less than 700 mg/day.
Limitations
This study also had some limitations. Less than half of the residents had a follow-up of more than 15 months. Nevertheless, a reduced risk was found after only 5 months. Furthermore, follow-up on the dairy intervention was monitored in 716 residents (10%).
Conclusion
Older adults often have an insufficient intake of protein and calcium. This study shows that increasing dairy consumption in older adults from 2 to 3.5 servings per day increases protein and calcium intake. A highly beneficial effect of the intervention is that the risk of bone fractures and falls in this vulnerable group of people is greatly reduced.
According to the authors, the study has broad implications for healthcare policies to prevent bone fractures in care settings and possibly beyond.
